Healthcare Leadership: Navigating in the era of complex adaptive systems
By Joaquín Azpilicueta, Academic Co – Director Advanced Leadership Program in Healthcare.
Healthcare systems worldwide face multifaceted challenges, ranging from demographic shifts and technological advancements to pandemics and economic constraints.
In the last 65 years, innovation has experienced a continuous acceleration, following Moore’s law, both in market reach and in market adoption. Such is the speed that we have a challenge understanding and managing the impacts.
The discrepancy in healthcare innovation adoption
Innovation in healthcare has the same high speed, relevance, and the high impact in our lives, but adoption is, again, very slow comparatively and stunningly uneven across “comparable” geographies.
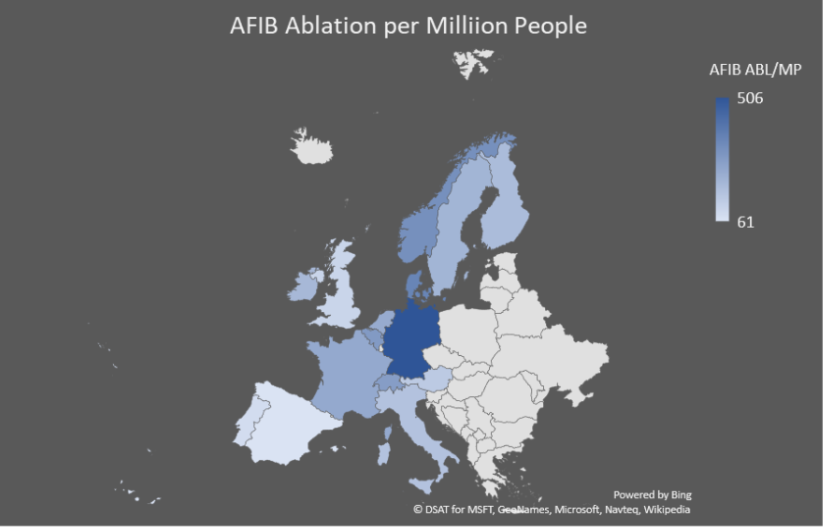
Understanding the variances in standard of care – An illustrative discrepancy
Let’s take an example of these asymmetries: the ablation of pulmonary veins is a standard of care therapy to treat atrial fibrillation, a widespread condition that represents a very high burden for every health care leadership system. This treatment is well depicted in the guidelines of the European Society of Cardiology, so the practicing cardiologists across Europe know when and how to treat patients with this condition that have a similar frequency (prevalence) across the geographies. This is a map of the indication rate of the therapy (number of patients treated per 1000 inhabitants. Source: ESC White Book 2016. At the time the guidelines were already published).
How can we explain that such a standard of care therapy has an indication rate 8.3 times higher in the highest indication country (Germany) as compared with the lowest (Spain) with high variability among the rest of Western European countries?
The digitalization lag in healthcare
Innovation has a major lever in digitalization that impacts many areas (information access, collaboration, data analytics, automation, digital platforms and ecosystems, customer centric innovations, IoT…) but are all industries equally developed?
If we look at healthcare, the penetration of digitalization is lagging any other industry by a magnitude of decades, especially in certain areas.
The atypical ecosystem of healthcare
Healthcare is a leadership ecosystem that differs from the ones we are used to dealing with in enterprise management. If we look at the classic facts of the “mystical” nature of a big part of healthcare delivery, the deep hierarchical culture and the information asymmetries between care giving professionals, the, patients and administrators, on one side, and the fact that the HC professionals are executives that don’t play a key role in the managerial processes, on the other side, we are in front of a very atypical enterprise model.
Challenges of healthcare leadership systems
Things are changing very quickly, or shall we say, “we want” things to change very quickly, but the adoption of innovations in healthcare takes ages to evolve and become standards of care, amid an amazing improvement in health metrics that happen with extreme asymmetries, as we have depicted before.
- Pressure: Govt. health care systems strained by economic, political, and demographic factors – HC budgets silo-ed & capped
- Adoption Barriers: block patient access to many innovating therapies
- Slow adoption of innovation: 17 years to standard of care (MedTech)
- Procurement systems: focus on cost, not value
- Physicians/patients: not sufficiently involved in access issues
- Patient empowerment: Rising consumerism, not medical literacy
- Minimal liability: if new therapies not adopted
Toxic behaviors in healthcare systems
HC systems show behaviors that are toxic, including:
- Cost shifting
- Bargaining power
- Capture patients and restrict choice
- Cost reduction through service restriction
- Locally focused
- Opacity
These behaviors hinder the development of value-based healthcare systems.
Transition to to leadership in value-based healthcare
Long ago we were wishing to build value-based healthcare systems that behave very differently (Porter, Michael E., and Elizabeth O. Teisberg. Redefining Health Care: Creating Value-Based Competition on Results. Boston: Harvard Business School Press, 2006.),
- Focus on value to patient
- Results based
- Medical conditions, disease management
- Cost reduction through quality
- Provider value through proficiency at the medical condition level
- Wider territorial competitive field
- Transparency
- Innovation to be strongly rewarded.
Shifting from benevolence to responsibility
Healthcare leadership systems have traditionally been based on benevolence, but this paradigm needs to evolve to a one based on responsibility. There are no “stakeholders” there are “agents”, parties that “act” and that need to coordinate their action to overcome the non-linearity of the healthcare systems, the “behavioral emergencies” of the systems that surprise with paradoxical outcomes. Not always for the bad though: during COVID we witnessed an amazing self-organization behavior that involved practically all the healthcare agents bringing the miracle of the chain of research, development, validation, production, distribution, administration, and vigilance of vaccines happening at speedlight.
The theory of complex adaptive Systems (CAS) in Healthcare
There were accelerating tools that helped, no doubt. In fact, they were determinant: digitalization, data management and communication for instance, what is referred to as “Digital-in-Health”. But this was there before, widely underused. Health care is lagging decades in the use of digitalization as compared to any other industry. The key during COVID was that agents minimized competition and maximized cooperation. Why? Because the situation was dramatic.
This level of criticality triggered a self-organization that produced the emergence of an “orchestrated” movement without a conductor, very much like the starlings that decide to turn, land, or take off all at once. This is a typical behavior of a Complex Adaptive System (CAS). The theory of CAS, with a focus on leadership, offers a conceptual framework to understand and manage the intricacies of healthcare ecosystems.
Core principles of CAS in healthcare
This theory of CAS, borrowed from complexity science, views healthcare as a system of interconnected and adaptive agents whose interactions give rise to emergent behaviours. Here are the core principles of these systems:
- Non-linearity and Emergence: Healthcare outcomes often arise from non-linear interactions among various elements. CAS theory recognizes the emergence of unexpected phenomena, providing insights into the unpredictable nature of patient responses to treatments and interventions.
- Self-Organization: CAS theory highlights the capacity of the system to self-organize, allowing for adaptation without centralized control. In healthcare, this implies acknowledging the autonomy of individual practitioners, departments, and even patients in decision-making processes.
- Feedback Loops: The existence of feedback loops in CAS influences system dynamics. Applying this principle in healthcare involves continuous learning through feedback mechanisms, such as data analytics and patient outcomes assessment, to refine and adapt strategies over time.
Applying CAS principles to healthcare challenges
Healthcare systems continuously show their adaptive capacity, most of the times not for the good though, considering the above mentioned asymmetries in care delivery. This capacity should be oriented to address the key challenges:
- Resilience to External Shocks: Healthcare systems must be resilient to sudden changes, such as disease outbreaks or shifts in patient demographics. CAS theory encourages the development of adaptive strategies to enhance the system’s ability to absorb shocks and recover.
- Innovation and Learning: The adaptive nature of CAS promotes a culture of innovation and continuous learning. Healthcare organizations can embrace this by fostering interdisciplinary collaboration, encouraging experimentation, and implementing flexible policies that adapt to emerging evidence.
- Patient-Centered Care: Recognizing patients as active agents within the healthcare system aligns with CAS principles. Empowering patients in decision-making processes and treatment plans acknowledges their role as adaptive entities with unique needs and preferences.
- Resistance to Change: The hierarchical nature of many healthcare systems can pose challenges to the decentralized and adaptive nature advocated by CAS theory. Overcoming resistance to change requires strategic leadership and cultural shifts.
- Cooperation through Data Integration and Interoperability: Effective adaptation in healthcare relies on comprehensive data integration. Challenges related to interoperability and data sharing must be addressed to realize the full potential of CAS theory.
The application of the theory of Complex Adaptive Systems in healthcare is a pillar of the leadership program.
Understanding the principles of CAS is essential for any executive agent in healthcare. It will be key to foster the adaptability, resilience, and innovation within healthcare systems, ultimately leading to improved patient care and outcomes, but also to the sustainability of healthcare systems as a whole and of every healthcare agent’s interest and progress.
Shaping collective leadership for value-based healthcare systems
While there are numerous commendable initiatives and leadership development courses focused on the immediate stakeholders within hospitals, often at the regional or national level, they tend to adopt a somewhat “domestic” approach.
In our newly developed course, the “Advanced Leadership Program in Healthcare”, we recognize two critical factors essential for driving significant change in healthcare leadership: embracing the entirety of the ecosystem and activating stakeholders. Stakeholders, defined as individuals, groups, or organizations actively involved or passively affected, play a pivotal role in this context.
Effective healthcare leadership necessitates fostering collaboration that transcends traditional boundaries. This involves establishing a shared vision, promoting unity, and ensuring unwavering commitment. Notably, patients, as the ultimate beneficiaries, assume a central role in navigating this dynamic landscape.
Key questions addressed in the Advanced Leadership Program in Healthcare
The program will address and answer the following questions in a practical way to provide the attendees with the value for money and to build the foundation of the program for its successful continuity:
- What are the forces that foster or oppose the pillars of adaptive capacity?
- How to overcome the resistances?
- Who and how should lead the positive interactions and avoid/relieve the frictions?
- What are the skills, strategies and tactics that are needed?
Why is the IE Business School and the King’s College developing this program?
Because it is a relevant, critical mission to boost and transform the leadership skills and behaviours of ALL healthcare agents. They are the ones responsible for a faster progress and even the survival of healthcare systems.
The agents cannot stay in their own house managing their own business with a “clan culture” disconnected from the rest, competing with the rest. They must find paths of collective leadership across boundaries to drive common direction, alignment, and commitment.
Why should all kind of leading healthcare agents attend? Because they will get exposure to and learn the skills, behaviours and strategies that matter to make their influence positive and effective resulting in their own and the collective benefit.
There is one agent that will for sure attend: Patients: we all are or will be patients, clients of the healthcare systems through our life. Patients are not stakeholders, we, patients, have our own responsibility to act in favour of healthcare, we need to understand and embrace our tasks. Making the healthcare systems better every day is the utmost incentive that should move all of us, regardless of what executive role we play.